P604
Calcium is required for a number of physiological processes, including bone formation, muscle contraction, cellular signaling, and nerve conduction. Because of this, the amount of calcium in the blood must be closely regulated between 8.5 and 10 mg/100 mL. The body has a sophisticated suite of hormones which maintain calcium homeostasis by influencing calcium uptake and release in the bones, gastrointestinal tract, and kidneys.
Parathyroid hormone (PTH) is a polypeptide hormone released from the chief cells of the parathyroid gland in response to low serum Ca2+ concentrations. The main effects of PTH include reducing the reabsorption of phosphate in the kidney, activating the breakdown of bone to release Ca2+, increasing Ca2+ reabsorption in the proximal kidney tubules. Conversely, high levels of plasma Ca2+ cause the release of the peptide hormone calcitonin (CT) from the clear cells of the thyroid gland. CT acts to promote bone mineralization through inhibiting osteoclast activity. CT also decreases Ca2+ reabsorption by the kidneys.
Vitamin D3, which acts in a similar manner to steroid hormones, functions to increase Ca2+ levels. It does this by promoting greater intestinal absorption of the mineral, increasing resorption of bone, and encouraging renal Ca2+ reabsorption. Vitamin D3 formation involves the skin, liver, and kidneys as outlined in Reactions 1 – 3.
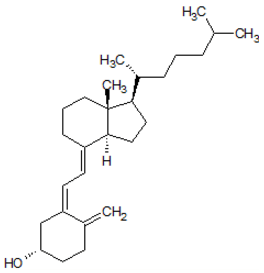
Figure 1. Structure of Vitamin D3.
Reaction 1
Cholecalciferol → 25-Hydroxycholecalciferol
Reaction 2
25-Hydroxycholecalciferol → 1-alpha-25-dihydroxycholecalciferol (Vitamin D3)
Reaction 3
Reaction 1 is induced by exposure of the skin to UV. Reaction 2 is catalyzed in the liver by 25-hydroxylase. Reaction 3 is catalyzed in the kidney via 1-alpha-hydroxylase. 1-alpha-hydroxylase is also the subject of tight regulation and is stimulated by PTH, decreased intake of Ca2+, and estrogen and prolactin during pregnancy.
.
Find an error? Take a screenshot, email it to us at error@mytestingsolution.com, and we’ll send you $3!
